Anyone
may
arrange his affairs so that his taxes shall be as low as possible; he is not bound to choose
that
pattern which best pays the treasury. There is not even a patriotic duty to increase one's
taxes.
Over and over again the Courts have said that there is nothing sinister in so arranging
affairs
as
to keep taxes as low as possible. Everyone does it, rich and poor alike and all do right,
for
nobody
owes any public duty to pay more than the law demands.
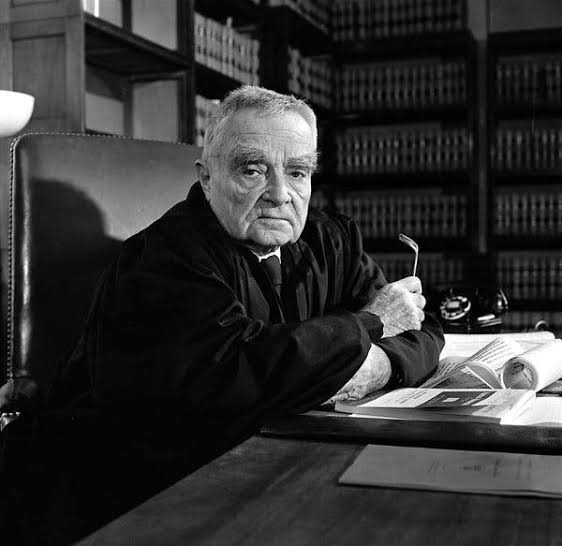
Judge Learned Hand
Chief Judge of the United States Court of Appeals
for the Second Circuit
Gregory v. Helvering, 69 F